For heel-valgus clubfoot, orthopedic shoes are made. Planovalgus deformity of the feet - we are looking for a good orthopedist. Attention! The project "Towards Life" provides an opportunity for free treatment
Congenital clubfoot- a malformation of the foot, characterized by its adduction, supination and plantar flexion.
Reasons There is a lot of clubfoot development. In one of the first places is the fusion of the amnion with the surface of the embryo's limb.
In addition, the reasons are the pressure of the amniotic cords or umbilical cord on the foot, the pressure of the uterus on the outer surface of the foot with a small amount of amniotic fluid; pressure by a tumor of the body of the uterus; toxoplasmosis in the mother; dysfunction of the spinal nerves; violation of the normal development of the lower extremities in the first 3 months of life, etc.
The clinical picture of clubfoot... There are plantar flexion of the foot in the ankle joint (equinus), rotation of the plantar surface inward with lowering of the outer edge (supination of the foot), adduction of the foot in the anterior section with an increase in its arch (adduction).
Deformity of the foot is combined with rotation of the lower leg inward at the level of the lower third and limited mobility in the ankle joint. When a child begins to walk, in the presence of clubfoot, there is a coarsening of the skin of the outer edge of the foot, atrophy of the muscles of the lower leg, especially the gastrocnemius muscle, and recurvation of the knee joints, as well as a peculiar gait, in which one foot is transferred through the other.
T.S.Zatsepin shares congenital clubfoot into two clinical forms: typical (75%) and atypical (25%).
With typical clubfoot distinguish: 1) a mild form (varus contracture of Osten-Saken), with it the skin is inactive, bony protrusions are determined mainly due to the head of the talus; 2) soft tissue form, when the subcutaneous fat layer is well developed, the skin is mobile, and there are no bony protrusions.
Atypical clubfoot develops due to the formation of amniotic constrictions, arthrogryposis, underdevelopment of the tibia.
Congenital clubfoot treatment should be started in newborns after the umbilical wound is overgrown. The essence of non-surgical treatment consists in repressive gymnastics, correcting foot deformity (3-5 minutes with breaks to massage the muscles of the foot and lower leg 3-4 times a day), and keeping the foot in a corrected position with a soft bandage (according to Fink - Ettingen).
Each time the foot position is reached must be fixed using the Fink-Ettingen method of bandaging with a flannel bandage 5-6 cm wide, 2 m long when the knee is bent at an angle of 90 °. They begin to bandage from the foot. The frequency of repetitions of manipulations with subsequent bandaging depends on the severity of the deformity (possibly up to 10 times a day).
After reaching hypercorrection of the foot, and in the case of a soft tissue form of its possible correction by the age of 2-3 months, to prevent relapses until walking is allowed, polyethylene splints are applied to hold the foot and lower leg in the hypercorrection position.
For moderate to severe clubfoot from 3 weeks of age, the child is treated with staged plaster casts. This is carried out directly by the orthopedic surgeon on a special table Nikiforova. Change of plaster casts and correction is carried out 1 time in 3 weeks without anesthesia. At night, the child needs to wear polyethylene splints.
At the same time, massage of the muscles of the lower leg and foot is prescribed., baths, corrective gymnastics, and with weakening of muscles - their faradization, in particular of the peroneal muscle group. In the absence of the effect of non-operative treatment in children from 6 months of age, operations on the tendon-ligamentous apparatus of the foot are recommended.
For severe forms of congenital clubfoot from the age of 3 years, surgery is indicated on the tendon-ligamentous apparatus according to T.S. Zatsepin with the use of a distraction-compression apparatus to bring the foot to the hypercorrection position, reposition the talus into the ankle fork and decompress the talus.
In 1951 V.A. Sturm proposed ligamentocapsulotomy- Surgical intervention on the ligamentous and tendon apparatus of the foot with the obligatory dissection of the capsule of the tarsometatarsal joints and the ligament between the scaphoid and I sphenoid bones. These operations are recommended for children under 10 years of age.
For severe clubfoot with pronounced adduction and supination of the foot in advanced cases, an operation is performed on the bones of the foot at the age of 12 years and older. This is a wedge-shaped resection of the foot bones with a base along the outer edge in the area of the calcaneo-cuboid joint and apex in the area of the talonavicular joint. Sometimes crescent resection of the foot bones is performed according to M.I. Kuslik and fixation with a distraction apparatus. This operation removes a crescent-shaped bone fragment in the midfoot.
Plovalgus foot.
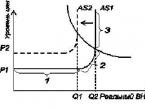
If the patient is not given regular treatment, then flat feet may progress and flat-valgus deformity of the foot will occur. In this case, the longitudinal arch is sharply flattened to the III degree, pain appears when walking rather quickly and is noted in the area of the inner ankle when the deltoid ligament is sharply stretched. The talus tilts and descends with its head and neck downwards. The plantar nerve passes under the head of the talus - an extension of the posterior tibial nerve.
Its trauma leads to neuropathy of the plantar and posterior tibial nerves. This causes a reflex spasm of the leg and foot muscles. The lateral heel bone presses on the lower pole of the outer ankle, also causing pain. The calcaneus is set in a sharply valgus position. When the arch is flattened, the forefoot is retracted outward.
Non-surgical treatment of planovalgus deformity of the foot
with the use of insoles-instep supports and orthopedic shoes with an external hard bristle is not always effective. The patient is shown to correct the deformity of the foot surgery.
The method of treatment according to F.R. Bogdanov consists in economical resection of the calcaneo-cuboid and talo-navicular joints for their arthrodesis in the corrected position of the longitudinal and transverse arches of the foot with simultaneous lengthening of the tendon of the short peroneal muscle, transplantation of the tendon of the long peroneal muscle to the inner surface of the foot under the heel - a scaphoid ligament, as well as lengthening the heel tendon with the elimination of heel pronation and abduction of the forefoot.
Method of treatment according to M.I. Kuslik
consists in sickle-transverse resection of the foot with lengthening of the calcaneal tendon and transplantation of the tendon of the peroneus longus muscle to the inner edge of the foot. After the operation, the patient must wear orthopedic shoes.
Clubfoot is a persistent deformity of the foot and ankle joint, congenital or acquired, in which a person cannot put the sole flat on the floor due to the fact that it is "turned" inward and bent at the sole, while the heel is lifted up.
The location of the bones, muscles and ligaments of the foot in this pathology is grossly impaired, the mobility in the ankle is sharply limited. All this leads to a violation of the musculoskeletal function of the lower limb and a specific gait - with support not on the entire sole, but only on its outer edge.
Most often, clubfoot is congenital, but it can be acquired and occur in adults as a result of injuries and other diseases of the musculoskeletal system, nervous system.
The congenital form of the pathology is 2 times more common in boys and, as a rule, is bilateral, in contrast to the acquired variants of the defect.

With clubfoot, the development of the bones of the foot, its muscles and ligaments is impaired
Classification
There are several options for the classification of this defect of the musculoskeletal system. Let's consider them in more detail.
As already mentioned, depending on the cause of the pathology, two groups of clubfoot are distinguished:
- congenital;
- acquired.
ICD-10 (international classification of diseases 10 revision) classifies clubfoot in the group of congenital deformities of the foot (Q66):
- Q66.0 Horse-varus clubfoot.
- Q66.1 Calcaneal varus clubfoot.
- Q66.4 Calcaneal-valgus clubfoot.
Speaking of clubfoot, most experts mean exactly varus deformities (when the sole is “turned inside out”). This pathology accounts for up to 85% of such defects. But there are also hallux valgus variants, when the foot bends outward. If the first option is diagnosed from birth, then the second becomes noticeable at the age of 1–1.5 years, when the child begins to walk.
The acquired variants of pathology are included in the category of acquired valgus (M21.0) and varus (M21.1) deformities of the foot.
It is important to understand that clubfoot is a collective term that includes not one disorder, but a whole group of foot deformities with its pathological setting.

Horse-varus congenital bilateral clubfoot in a child

Heel-valgus congenital clubfoot in a child
Depending on the severity of the pathology, there are:
- Mild degree - in this case, clubfoot can be corrected at home, pathological changes in bones are minimal, mobility in the ankle is not impaired. All symptoms are easily eliminated with massage and exercise therapy.
- Moderate severity- It is possible to completely remove the clubfoot, but this requires the professional help of a pediatric orthopedist. As a rule, the treatment is conservative. In this case, there is a lesion of the ankle joint and more pronounced deformities of the skeleton of the foot, underdevelopment of muscles and ligamentous elements.
- Severe degree - to correct such a clubfoot is possible only by surgery. In this case, pathological changes in the foot and ankle joint are pronounced.
- Very severe- unfortunately, it is almost impossible to cure such a pathology even with the use of modern methods of surgical correction. A child can remain disabled for life.
Classification according to Zatsepin, who proposed to divide all types of congenital clubfoot into two groups.
Typical (or primary):
- mild varus contractures;
- ligamentous (soft tissue) forms;
- bone forms.
Atypical (secondary):
- neurogenic form (caused by diseases of the nervous system);
- amniotic (damage to the baby's foot by amniotic constrictions during intrauterine development);
- against the background of defects in the development of bones (for example, due to underdevelopment of the tibia);
- against the background of arthrogryposis (a serious congenital disease, which is accompanied by damage to almost all joints in the child's body).
It is the Zatsepin classification that is used today by most orthopedists in the world.

Clubfoot is one of the signs of arthrogryposis
You can also often find a variant of the classification of congenital clubfoot Ponseti:
- untreated - a congenital or acquired form of pathology in a child under 8 years old, which did not respond to any therapy;
- corrected - cured by the Ponseti method;
- recurrent - despite the presence of a full range of appropriate measures, the progression of the defect continues;
- resistant - it is established when clubfoot is combined with other serious diseases, due to which its correction is almost impossible, for example, with arthrogryposis;
- atypical.
Causes
The congenital form of the disease is polyetiological, that is, there are many negative factors that can cause the development of this form of foot deformity in a child. They can be divided into several groups:
- Mechanical effects - incorrect position of the fetus inside the uterus, amniotic constrictions.
- Neuromuscular disorders - abnormal development of the muscle and ligamentous components of the foot, which leads to the development of deformity.
- Toxic factors - the impact on the child's body during the period of intrauterine development of various medications, other chemicals.
- Genetic - there is also a hereditary theory of clubfoot, but, unfortunately, the pathological gene has not yet been identified.
The congenital form of pathology can be one- or two-sided, be an independent disease or be combined with other malformations and ailments.
The acquired form is diagnosed in adults. It can develop due to:
- pathological union of fractures in the foot and ankle;
- damage to soft tissues due to deep burns;
- diseases of bones and joints (osteomyelitis, rickets, arthrosis, arthritis, tumor lesions);
- neurological diseases (with brain damage and the development of central types of paralysis);
- ailments that are associated with impaired bone growth;
- increased loads on the lower limbs;
- obesity;
- choosing the wrong shoes.

Shoes for the child need to be orthopedic, otherwise the risk of developing acquired clubfoot increases
Symptoms
Clubfoot is usually easy to recognize on examination. Additional diagnostic methods help to establish the degree of disorders, the cause and form of the disease.
Congenital variants
Varus forms differ in the pathological setting of the foot immediately after birth. One or both legs are in a state of plantar flexion (equinus), with the foot turned in such a way that the sole looks back (supination) with adduction of the anterior section (adduction). These 3 symptoms (equinus, supination and adduction) are pathognomonic symptoms of congenital clubfoot.
Additional signs to help diagnose the problem:
- the heel is raised up, and the forefoot is lowered and directed down;
- the foot is unusually small;
- there is an Adams groove on the sole;
- limited mobility in the ankle;
- the axis that passes through the heel bone is displaced relative to the axis of the lower leg (they normally coincide).

Adams groove on the sole of a child with congenital clubfoot
Purchased options
This type of pathology, as a rule, develops in children aged 3 years, adolescents and adults for the reasons described above. In this case, the following symptoms gradually develop:
- change in the usual gait ("bear gait" - when walking, the patient, as it were, "rakes" with one or two legs);
- convergence of the knee joints and the development of an X-shaped deformity of the lower extremities;
- decreased mobility in the ankle;
- acquisition of the hallux valgus by the first toe.

Acquired valgus clubfoot in an adult
It should also be noted that the acquired forms of deformity are most often of a valgus nature, that is, with a deflection of the foot to the outside.
Diagnostics
The congenital variant of the disease can be diagnosed even during the intrauterine development of the child using ultrasound. The defect becomes noticeable already at the 19th week of pregnancy. If clubfoot is not recognized before the birth of the baby, then this is easy to do when examining the newborn immediately after birth.
The acquired form can be suspected by the signs described above and on examination by an orthopedic surgeon.
X-ray, CT, MRI, ultrasound will help to confirm the diagnosis.
It is important to note that an X-ray is not always informative, especially for small patients. In children, the bones of the foot are not yet fully formed; their part is formed by cartilaginous tissue, which is not visible on x-rays.
Possible complications
If the problem is not recognized in time and treatment is not started, the deformity can progress, and complications can develop over time. It is generally accepted that the pathology must be eliminated up to a year, until the child begins to walk, since under the influence of load during steps, the deformation will progress.
Possible complications:
- scoliosis and other deformities of the spine due to the pathological position of the feet;
- atrophy of muscles and ligaments of the lower limb;
- violation of gait, inability to move independently;
- lag in the physical development of the baby;
- dislocations and subluxations of the feet, knee and hip joints;
- pathology of the knee and hip joints;
- persistent pain syndrome.

In some cases, congenital clubfoot does not respond to treatment and can cause permanent disability in the child.
How to get rid of clubfoot
Clubfoot can be cured. For this, various conservative and surgical techniques are used. This problem is dealt with by an orthopedic surgeon. The earlier the problem is recognized and therapy is started, the better the prognosis.
Ponseti Clubfoot Treatment (Casting)
This method of conservative treatment of clubfoot was developed by Ignazio Ponseti in the USA in the 1950s. The specialist was against the surgical correction of the defect, as he believed that such an intervention leads to secondary gross disorders, which often prevents the normal function of the child's foot and ankle from being restored.

The Ponseti Method is an effective conservative treatment for clubfoot with high performance
After a detailed analysis of the physiology and biomechanics of the foot, the doctor proposed a new method of plastering, which can be started at any age, but preferably from two weeks.
Usually, after 5-6 casts, it is possible to completely correct the deformation. Typically, the entire course of treatment takes 4-8 weeks.
After the end of the cast, the child must wear a special orthopedic fixator (brace). The main task of the brace is to stretch the muscles, which will help prevent relapses. It is very important to adhere to the prescribed mode of wearing the orthopedic brace. According to statistics, only 6% of children whose parents adhere to the brace regimen have a relapse of clubfoot.

Congenital clubfoot brace
Other methods of conservative treatment
Soft bandages
This method is close to the previous one, but fixation is carried out with bandages. The method can be used with a slight degree of deformation in combination with a set of therapeutic exercises and massage.
Elastic orthopedic structures
These tires and splints are made from special metal alloys. Although they are gentle, but securely fix the feet in the correct position.
Orthoses
The technique consists in fixing the feet and ankles in the desired position using special orthopedic orthoses. This group of therapeutic effects includes orthopedic shoes, insoles, rigid splints, elastic orthoses.
Massage
It is an indispensable component of conservative treatment. Only a specialist should massage the feet and legs. As a rule, you need from 4 to 10 courses of special manual influence.

Therapeutic foot massage of a child should be done only by a specialist.
Physiotherapy
Exercise therapy also plays an important role in the correction and prevention of recurrence of clubfoot. You need to work with your child every day. The exercises must first be learned with a doctor, and in the future you can do them yourself at home.
Physiotherapy procedures
Physiotherapy is an auxiliary method of therapy and can be used in children over 2 years of age. Most often, magnetotherapy, electrophoresis, phonophoresis, and warm paraffin applications are prescribed.
Medicines
Play a minor role in treatment. Vitamins, especially of group B, can be used. Also, depending on the cause of clubfoot, the doctor may prescribe one or another medication course of treatment.
Surgical correction
The operation is resorted to only in cases where clubfoot was diagnosed late and conservative therapy did not give a positive result. Also, surgical correction is prescribed in difficult cases when the defects are very severe and cannot be eliminated by usual methods.
Clubfoot is a serious defect of the musculoskeletal system, especially its congenital forms. But in the case when the problem was noticed on time, and the treatment was prescribed correctly, clubfoot is quickly and easily eliminated, and the child will begin to walk correctly and without any difficulty.
Clubfoot is one of the orthopedic problems arising at the stage of formation of the child's musculoskeletal system in the first years of life.
Such an ailment can drastically change the quality of a baby's life and create the risk of developing serious problems in adulthood.
Clubfoot treatment prognosis depend on the degree of progression pathology and the reasons that provoked its appearance. It is necessary to correct the ailment when identifying its first signs. We will tell you about the treatment of clubfoot in children in the article.
How to do massage for muscle hypertonicity in a child? Find out from our.
Concept and characteristics

In medical practice, clubfoot means the provoking wrong position and deviation to the inside.
The disease can be not only congenital, but also acquired... With clubfoot, serious deformation occurs not only of the bones, but also of the muscle tissue. In most cases, the pathology affects both legs of the child.
Causes of occurrence
Numerous factors can provoke clubfoot, including pathologies associated with with intrauterine development of the fetus.
The disease is a consequence of improper formation of the bone skeleton, muscle tissue and joints.
In some cases, the pathological process is a consequence of a violation of the state of certain groups of nerves or blood vessels. In medical practice, there are cases when the causes of clubfoot in a child cannot be established.
The reasons clubfoot can be caused by the following factors:

Disease classification
Depending on the stage of progression of the disease, clubfoot is subdivided into mild, moderate and severe... The first form is characterized by minor changes in the musculoskeletal system.
The second stage is accompanied by more intense symptoms and difficulty in moving the ankle joint.
A severe degree is characterized by a pronounced pathology and is eliminated only by the method of surgical intervention.
Other types of classification of clubfoot in children:

Symptoms and Signs
Symptoms of congenital clubfoot appear in a child already in the first months of life. Signs of the disease are clearly visible visually, due to which a suspicion of a pathology may arise in parents before a routine medical examination of a newborn or baby.
Symptoms of acquired clubfoot can occur in a toddler during the first year of life or during preschool age.
Clubfoot is accompanied by the following symptoms:
- external underdevelopment of the legs;
- in the plantar direction there is a characteristic curvature of the foot;
- a deep transverse fold is clearly visible on the baby's foot;
- the toes are bent towards the inner side of the foot;
- excessively in a newborn or infant;
- torsion of the lower leg on one or two legs;
- on foot.
Clubfoot in children - photo:

Consequences and complications of the disease
With clubfoot, a child gets used to putting the foot in a certain position... In the process of treating the disease, this habit must be eliminated.
If the child continues to walk in his usual manner, then it will be extremely difficult to correct his gait.
Clubfoot treatment in children should be comprehensive. With the wrong therapy or its absence, there is disability risk at the baby.
The consequences clubfoot in children can become the following conditions:
- curvature of the legs;
- flat feet;
- lag in physical development;
- rachiocampsis;
- disability.
How to fix clubfoot in a child? Treating congenital clubfoot in children, you can learn from the video:
We kindly ask you not to self-medicate. Make an appointment with a doctor!
The main task of the foot is to maintain body weight. It also acts as a kind of shock absorber. And therefore, as soon as a problem appears (injury or illness), then a person immediately ceases to enjoy life.
The state of deformation of the foot with the loss of its function and violation of the arches is called flat feet. In this case, people of all ages fall into the risk zone. According to statistics, the disease develops in a significant part of the world's population - more than 40%. Most of them (about 90%) are female.
Longitudinal and transverse flat feet is a serious condition that causes significant discomfort, interfering with normal walking. Patients also cannot get on their feet painlessly. Therefore, everyone is interested in the question: is it possible to cure flat feet?
Causes
Anatomically, the human foot has a transverse arch (it is located directly under the toes), longitudinal (it runs along the edge). With deformation, the load is redistributed between the spine and leg joints. As a result, a person has serious problems not only with his legs, but also with his back. To avoid unpleasant consequences, it is advisable to start treating transverse, longitudinal flat feet in time.
Causes of flat feet:
- Heredity.
- Weak ligaments, as well as the muscles of the foot.
- Being overweight.
- Pregnancy.
- Work activity associated with excessive loads.
By the nature of occurrence, the following types of flat feet are distinguished: acquired, congenital. In most patients, the disease is acquired.
Disease in children
Congenital flat feet are associated with impaired fetal development in the prenatal period. This type of disease is rare. Children are already born with flat-valgus feet. Violation can be caused by oligohydramnios during pregnancy, taking certain medications, exposure to harmful radiation.
After birth, all babies will have a flat foot. The completion of the formation of its vaults takes about four years. Therefore, starting only from this age, doctors can make a similar diagnosis and begin treatment for flat feet.
If both parents suffer from congenital flat feet, then such children have a high risk of being born with such a pathology.
Therefore, it is necessary to carefully monitor the development of the child's foot in order to detect violations in a timely manner.
One of the signs of possible flat feet in the future is clubfoot in children. Pronounced congenital flat feet can be distinguished by the shape of the foot. In this case, the sole will be in contact with the surface over a large area. In addition, there are the following distinguishing features:
- Gait disorder.
- Tired legs.
- Swelling in the leg and foot.
- The child has difficulty maintaining balance.
- The muscles of the lower leg are disproportionate.
Since the signs appear gradually, it is almost impossible to identify flat feet in children at the initial stages. But the success of treatment will depend on how early this pathology was detected.
Congenital flat feet, which is inherited, cannot be completely corrected. Treatment in such cases consists in strengthening the muscles and ligaments of the musculoskeletal system. Prevention is also just as important.
Illness in adults
Acquired flat feet are usually caused by weakening of muscles, ligaments, and bone deformation. Such flat feet are called static. The disease can also provoke a fracture of the ankle, fracture of the calcaneus and tarsal bones, ankle, as well as other injuries not only of the arch of the foot, but of soft tissues.
Another reason for the development of flat feet in adults can be called rickets, transferred in childhood. With this disease, the framework of the foot weakens, and therefore is not able to withstand the load of the body. As a result of this, deformation of the bones that are in the foot occurs, that is, flat feet appear.
Symptoms

The clinical manifestations of flat feet depend on several factors: the severity of this disease, as well as on how strong the changes that have occurred. Mild dysfunction of the feet, as evidenced by fatigue in the legs in the evening, is an early stage (otherwise it is called latent). In such cases, there are no visual signs of deformation.
Doctors distinguish 3 degrees of severity of this disease:
- Grade 1 is expressed in the presence of mild pain, which occurs if you even stand a little on your leg or press lightly on any area of the foot. Also in the evening, you may notice swelling in your legs, which goes away on its own after sleep.
- 2 degree of flat feet is determined by the sign of flattening of the arch. Please note that in such cases, the vaults are practically not rendered. As a result of the disease, significant difficulties arise not only during running, but also during normal stride. In addition, the painful sensations extend completely to all legs, the pain is pronounced and prolonged.
- Grade 3 - feet with pronounced deformation. When walking, a person experiences severe pain in the legs, which causes certain inconveniences. One of the signs can also be considered that the usual shoes are no longer suitable for wearing. With a 3 degree flatfoot, they are exempted from military service.
Since the disease develops rapidly, it is recommended that at the first suspicion of flat feet, seek medical attention from a doctor. He will prescribe treatment to prevent possible complications. As such, arthritis, hernia, curvature of the spine can become.
Often, the symptoms of flat feet in the early stages do not appear in any way, which is why a person confuses them with other diseases that affect the condition of the lower extremities. It all starts with the fact that he feels tired and unwell in his legs. After a while, pains appear, which become so strong that they radiate to the spine. The very shape of the foot also changes: the “bump” bone at the base of the big toe increases, as a result of which it deforms and changes its position - it goes under the second toe.
Constantly forming calluses and calluses on the foot are also referred to as symptoms of flat feet. The disease is also characterized by the inability to stand on tiptoes.
Symptoms of flat feet also appear, such as:
- Shoes wear out prematurely (especially the inner part), change their shape.
- When walking on stiletto heels or high heels, a woman's foot begins to hurt. Soreness also occurs if you stand for a long time.
- Exercise more than usual provokes pain in the lower extremities.
- In the evening, the legs will be swollen, sometimes cramps appear.
- The gait becomes clubfoot.
- The leg increases in length and width.
- Headaches and low back pain appear.
- The toes change their shape and length.
- The ankle and hip joints are deformed.
In children, a common manifestation of flat feet is fatigue, pain in the legs. As a result, spinal curvature or even arthrosis may occur. With flat feet, some children complain of headaches.
Kinds

In orthopedics, certain types of flat feet are distinguished. By the type of violation of the vault, it is classified into:
- longitudinal-transverse flat feet (combined);
- transverse flat feet;
- longitudinal flat feet.
Moreover, doctors say that in their practice, patients with transverse flat feet often come.
The diagnosis of "Longitudinal flat feet" is made if the patient complains of fatigue quickly arising in the legs. In addition, pain will appear when you try to apply even light pressure to approximately the middle of the foot. Swelling of the foot from the back is visualized.
Longitudinal flat feet, among other things, are expressed by constant severe pain, which is localized in the ankle joint. In some patients, pain is radiated to the lumbar region. The ankle joint becomes motionless, the foot itself swells - this leads to difficulty walking. Patients complain that there are big problems with the selection of comfortable shoes.
Transverse flat feet, if adequate treatment is not started in time, will lead to serious complications. In particular, there are pains in the kneecaps, pathology of the spine.
Symptoms by which you can recognize the transverse flat feet:
- The pain occurs throughout the foot, but it is more intense in the front.
- Coarseness of the skin on the outside.
- Deformation of the fingers.
- The transverse arch is smoothed at the foot.
When the disease progresses to the final stages, you can notice a slight increase in the size of the legs, not only in width, but also in length.
The gait changes - it becomes clumsy and heavy. Some patients find it difficult to maintain balance. As a result of circulatory failure, the skin on the foot begins to acquire a purple-blue hue. This type of flat feet is formed as a result of deformation of both arches of the foot.
Combined flat feet are characterized by the same symptoms as both previous types, only they are more pronounced. In addition to the soreness of the foot, it is characterized by swelling of the ankles, pain in the knees, back. Lameness and blueness of the skin of the foot also appears.
Diagnostics

The basis for the diagnosis is clinical presentation and examination. Moreover, the doctor must examine the patient's foot not only, but also the shoes - the shoes wear out in a characteristic way. In addition, the color of the skin of the foot, the presence of corns, seals and calluses are important.
With a healthy foot, the skin will be pinkish. If it has a purple-bluish tint, then this indicates venous stasis. If the color is pale, on the contrary, it indicates insufficient blood circulation.
There are also instrumental diagnostic methods:
- Podometry. It is used to determine the index of the arch of the foot (for this, the foot is measured). The result is estimated as a percentage. If there are no problems, then the index of the longitudinal vault will be in the range of 29-31%, but the transverse vault will be a maximum of 40%.
- Podography. Not only the biomechanics of walking is studied - the parameters of the foot movement are also considered in the diagnosis. This method allows you to analyze a person's gait, study the features of foot rolls and calculate the coefficient of gait rhythm.
- By means of radiography, abnormalities in the foot are assessed, and the degree of flat feet is determined. In addition, X-ray examination is used to monitor the treatment process in order to trace the dynamics of the disease.
- Electromyography is a method for diagnosing the condition of the ligamentous-muscular apparatus of the foot. It is very effective, since the severity of the disease depends on the condition of the muscles of the lower leg and foot.
- Pantography. When it is carried out, a footprint is left on special paper. To do this, specialists paint the lower part of the foot with various substances, and only then they make an imprint. This method makes it possible to find out in what state the arch of the foot is. If there are some suspicions, then using other methods, additional examination will be carried out.
It will be possible to diagnose pathology in children using plantography - this is obtaining a foot print, on which the points of load distribution will be marked. Diagnosis with an X-ray is not prescribed for children until they reach 4 years of age.
Treatment

People with a similar diagnosis have natural questions: how to treat flat feet? How to cure flat feet without surgery? What are the chances to correct the pathology completely? Doctors believe that the treatment of flat feet and its success will depend on how early it was detected, that is, on the stage of the disease.
Treatment of flat feet in adults and children should pursue 3 main goals:
- Relief from pain.
- Restoration of the functions of the foot impaired during the disease.
- Strengthening muscles and ligaments.
You can correct the foot in 2 methods: conservative, surgical. Moreover, the operation is resorted to only in cases of severe deformity of the feet.
To cure the disease completely, today's medicine does not allow. Therefore, all treatment is aimed at preventing further development.
Also, prevention will not hurt, especially if a person has a tendency to flat feet.
Conservative methods

As part of conservative treatment, various medications and procedures are prescribed - physiotherapy, massage, therapeutic exercises. In addition to these, it is recommended to wear special shoes and insoles.
The massage is especially effective in the early stages. It helps relieve pain and improve blood circulation.
Performing special exercises is advisable for the first degree of flat feet. With the help of exercises, you can correct the violation of the ratio of the bones of the foot and strengthen the muscles and ligaments. Classes should be regular. The recovery will be long.
As a physiotherapy, shock wave therapy, paraffin applications and electrophoresis are used. They are prescribed at all stages of the disease, are especially effective in case of pronounced pain syndrome and impaired mobility of the joints. With the help of these procedures, the mobility of the feet is restored, blood circulation and metabolism in tissues are improved. Physiotherapy should be used in combination with other methods of treatment.
Drug therapy will only help relieve pain. As such, it does not give efficacy to prevent the development of the disease.
Surgical methods for treating flat feet are used when other methods are ineffective and in a severe course of the disease, which is accompanied by complications.
Prophylaxis

If there is a risk of such a disease in children, then as a preventive measure it is necessary to purchase special orthopedic insoles or orthopedic shoes. It is equally important to monitor the nutrition of children. It should be fortified with vitamins, as well as phosphorus and calcium.
Scientists have proven that among adults, even with a hereditary predisposition to the disease, flat feet occurs 3 times less often if they spent a lot of time barefoot in childhood. That is, walking barefoot on the grass is an effective prevention.
Orthopedic insoles and shoes are recommended by specialists at the first sign of illness. Also, they will not harm women during pregnancy, athletes and persons who, by virtue of their profession, are on their feet for a long time. This method of treatment is at the same time a method of prevention. It helps to return the deformed foot to its normal position.